Thumb arthritis is a common cause of thumb pain. At the base of the thumb is a specialized joint called the thumb carpometacarpal (CMC) joint. This joint normally allows for a wide-range of thumb motion. The ability to touch the thumb to the small finger, known as “opposition,” is a function which distinguishes our hands from the hands of many animals. Because of this joint mobility, the base of the thumb is exposed to a large amount of “wear and tear” stress. Over time, this joint can “wear out” or become arthritic. The normal smooth cartilage wears away, leading to “bone-on-bone” contact. This can result in pain, weakness, and decreased thumb range of motion. Previous injury and family history of osteoarthritis may also contribute to this.
Thumb CMC joint arthritis is a common form of degenerative joint disease, also known as osteoarthritis. It is one of the most common places to get osteoarthritis in the hands. We use our thumbs for just about everything. Osteoarthritis is more common the older we get, and it is part of the usual aging process.
How do I know if I have thumb arthritis?
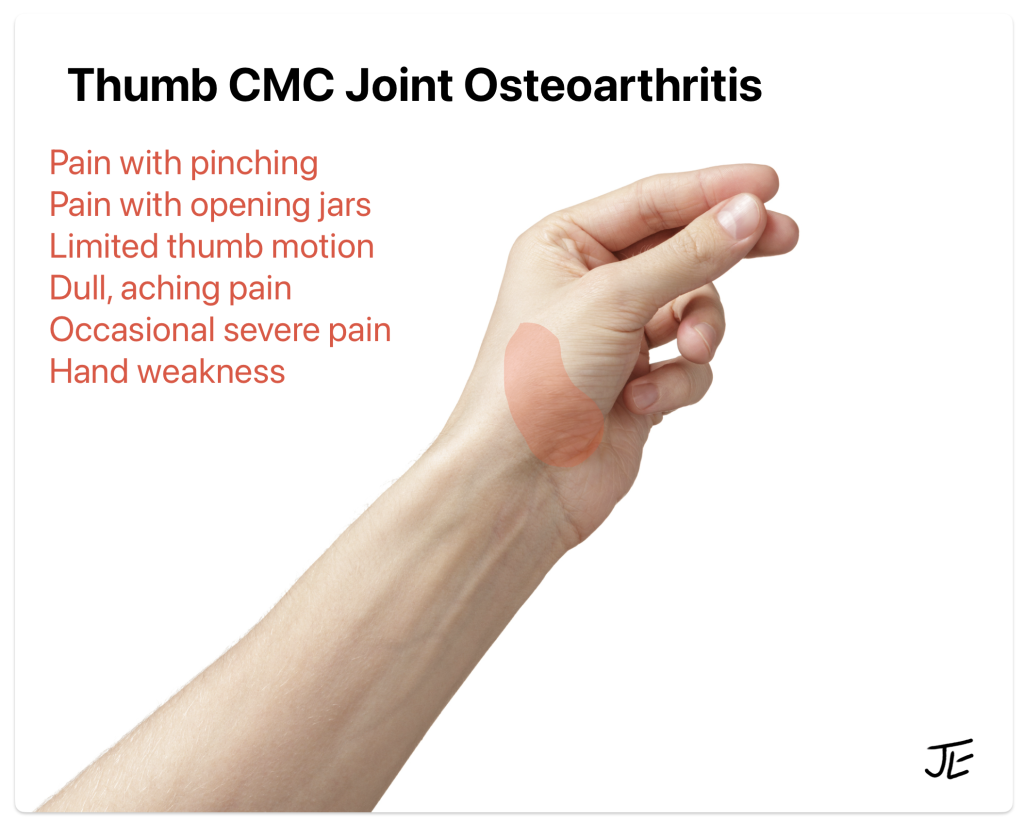
Most people notice a gradual onset of symptoms over time. Pain is usually located at the base of the thumb, but may radiate into the wrist, forearm, or hand. At first the pain may feel like a dull “ache” but it may become worse over time. Occasionally, sudden “sharp” pains can occur in the thumb. Activities such as opening a jar, turning door knobs, knitting, or using a key can be painful. Some people feel that they do not have the strength they used to have in the hand. Some people notice swelling or a bump at the base of their thumb, which may be painful to the touch.
How is thumb CMC joint arthritis diagnosed?
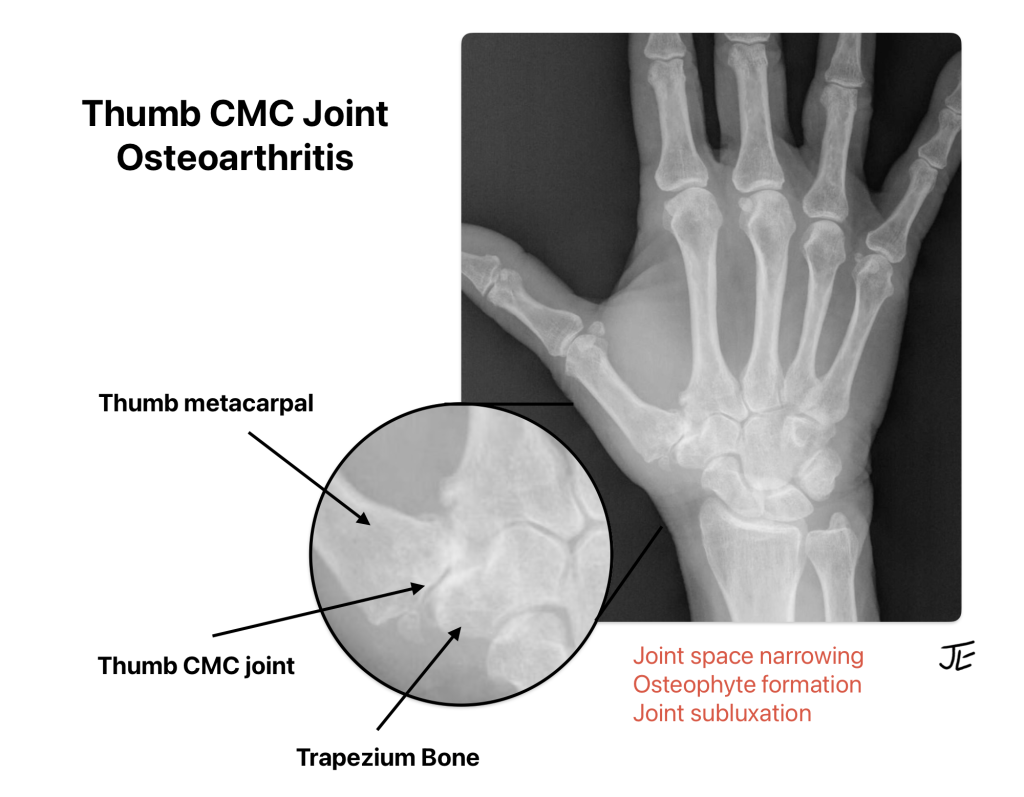
The diagnosis is made after reviewing the patient’s history, performing a physical examination, and getting x-rays. X-rays can show loss of joint cartilage, joint deformity, bone spurs (also called “osteophytes”), subchondral cysts within the bone, and narrowing of the joint space.
What are the treatment options for thumb arthritis in Raleigh?
There is no cure for osteoarthritis but the symptoms can be relieved. Non-operative treatment is usually helpful for most patients. Over-the-counter anti-inflammatory medications such as Naproxen (Aleve), Tylenol, and Ibuprofen (Motrin) can help reduce the pain. A thumb brace is often helpful during activities. Occupational therapists can also make a custom brace or thermoplast splint. Steroid injections (cortisone shots) into the thumb CMC joint can reduce pain temporarily. Turmeric arthritis supplements may reduce inflammation and pain in patients with hand osteoarthritis. These supplements are sold over the counter without a prescription. Some patients find relief from topical heating pads, warm water soaks, or topical anti-inflammatory lotions such as Voltaren gel.
Non-operative treatments for thumb arthritis:
- Thumb brace
- Oral anti-inflammatory medications (NSAIDs)
- Tylenol
- Turmeric supplements
- Topical medications and creams
- Cortisone injections
- Modifying activities
When non-operative treatment has failed to reduce symptoms to a manageable level, surgery may be offered. The decision to undergo surgery is based primarily on your symptoms and quality of life. Many patients can avoid surgery with adjusting their activities, using oral or topical medications, and using a thumb brace.
What surgery is recommended for thumb CMC arthritis?
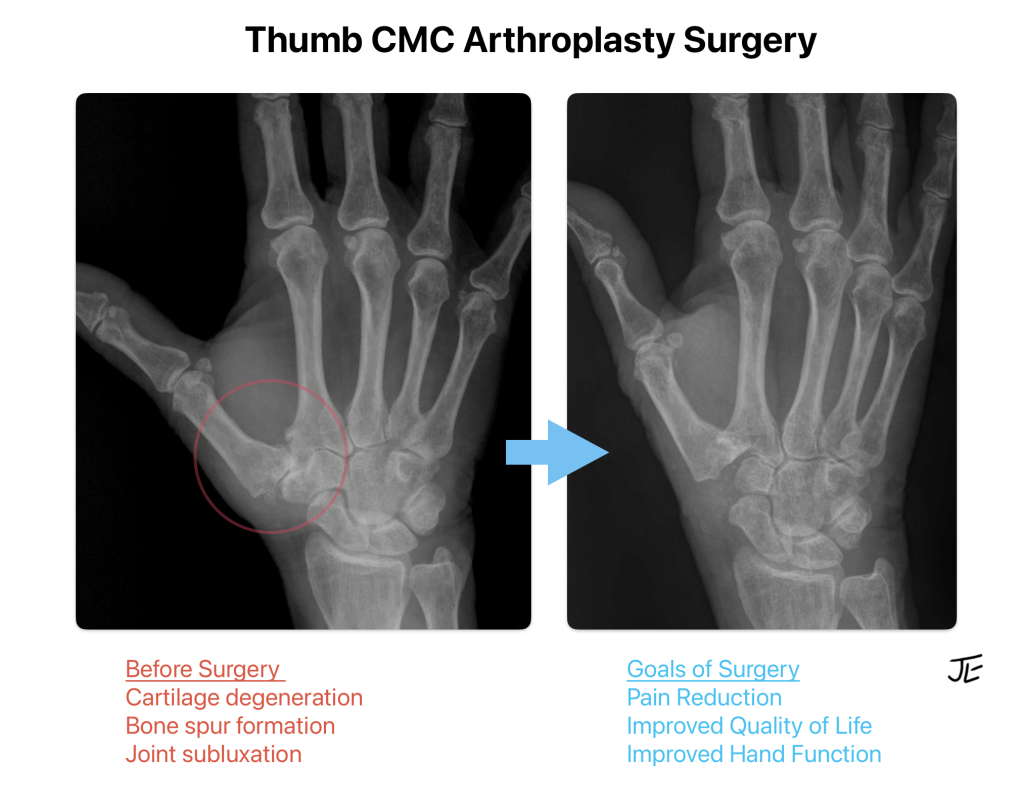
Thumb CMC arthroplasty surgery is a commonly performed hand procedure. The surgery is performed on an outpatient basis. General anesthesia can be avoided by using a temporary nerve block (regional anesthesia). During surgery, the arthritic bone at the base of the thumb (trapezium bone) is removed. This procedure eliminates the bone-on-bone grinding pain. In addition, a tendon from the patient’s forearm can be used to fill the space at the base of the thumb and/or reconstruct the ligaments at the thumb base. This tendon acts as a biologic spacer or cushion for the thumb. Alternatively, a strong suture can be used to stabilize the base of the thumb in a procedure called suture suspension arthroplasty. These options will be discussed with you in the office.
In this case, the bone spurs and lack of joint space can be seen at the base of the thumb, shown by the red arrows on the x-ray. This is what “bone-on-bone” arthritis looks like before surgery. Most patients regain good thumb range of motion and have significant pain relief.
What are the results from thumb arthritis surgery?
Thumb arthroplasty has been performed with excellent results since the 1940s and was popularized in the 1980s. This surgery has a proven track record in published studies with good long-term outcomes for the majority of patients. Most patients report less pain, improved grip strength, and better function after surgery.
What are other surgical options for thumb arthritis?
Some surgeons insert artificial or manufactured implants such as metal, silicone, or fiber in the base of the thumb. This introduces the risk of implant loosening, breakage, and rejection. Using artificial joint replacement implants has not been shown to be superior to traditional surgery. Therefore, I do not recommend these procedures.
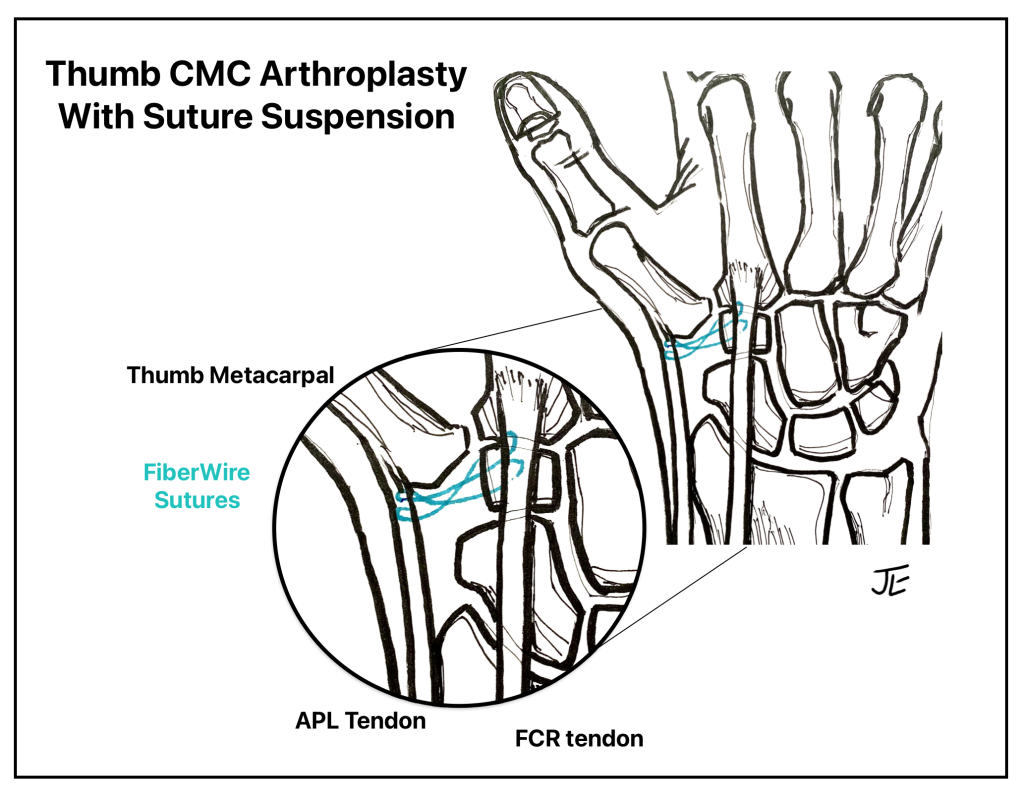
While I have performed the traditional tendon graft procedure for many years with good results, I have begun using the newer, less-invasive suture suspension technique. I believe that this newer technique is less painful and allows for a quicker recovery, compared to the traditional thumb surgeries. The suture suspension technique also has a low risk of complications and positive long-term outcome data. Recently published studies show good-to-excellent functional results in patients up to 14 years after suture suspension surgery, with improved pinch strength and maintained pain relief.
However, I advise patients that thumb surgery is not a “quick fix” as it takes about 3 months to return to heavy hand use. It can take up to a year to obtain maximal thumb range of motion and pinch strength after surgery. I also recommend that patients attempt several months of nonsurgical treatment before considering thumb surgery, since the symptoms may improve significantly without surgery.
Suture Suspension Thumb CMC Arthroplasty
Suture suspension arthroplasty is a newer technique which is becoming more popular as a less-invasive surgical option. After the trapeziectomy is performed, the surgeon uses strong sutures, often fiberwire, to stabilize the thumb base to the adjacent tendons. This technique does not require a drill hole in the bone or removal of a patient’s tendon. The procedure allows for early range of motion with hand therapy.
What can I expect after thumb arthritis surgery?
Your wrist and thumb will be protected in a plaster splint after surgery. This is removed in clinic along with the stitches after 2 weeks. At this point, patients are provided a custom-made splint which they wear for an additional 4 weeks. I recommend avoiding heavy use of the hand or strengthening for approximately 6 weeks after surgery. Hand therapy is helpful to improve range of motion and strength during the recovery.
This procedure is not a “quick fix” but more like an “investment.” Thumb arthritis surgery recovery can be painful at first and hand therapy is important to help with the recovery. Patients should expect about a 3 month recovery time period and up to a year for increasing range of motion and strength. The good news is that the majority of patients are satisfied with the results of surgery and are happy with the pain relief.
Patients can trust the doctors and therapists at Raleigh Hand to Shoulder Center to provide them with compassionate and effective treatment for their thumb arthritis in Raleigh.
Updated December 2025
Disclaimer: Please note, the material provided on this site is intended for general information only and does not constitute medical advice. This does not replace evaluation by a doctor. Please seek medical evaluation if you have a concern.

