Thumb CMC joint osteoarthritis is one of the most common problems which can affect our hands. We use our thumbs for many daily tasks including buttoning a shirt, opening a jar, and turning a doorknob. The ability to move the thumb to touch the small finger is an important function which makes the human hand unique. This function is made possible by the special anatomy of the thumb carpometacarpal joint, or simply the “thumb CMC joint.” However, this everyday motion and common hand activity can result in “wear and tear” in the joint. Over time the joint cartilage can degenerate, bone spurs can form, and there can be bone-on-bone grinding at the joint.
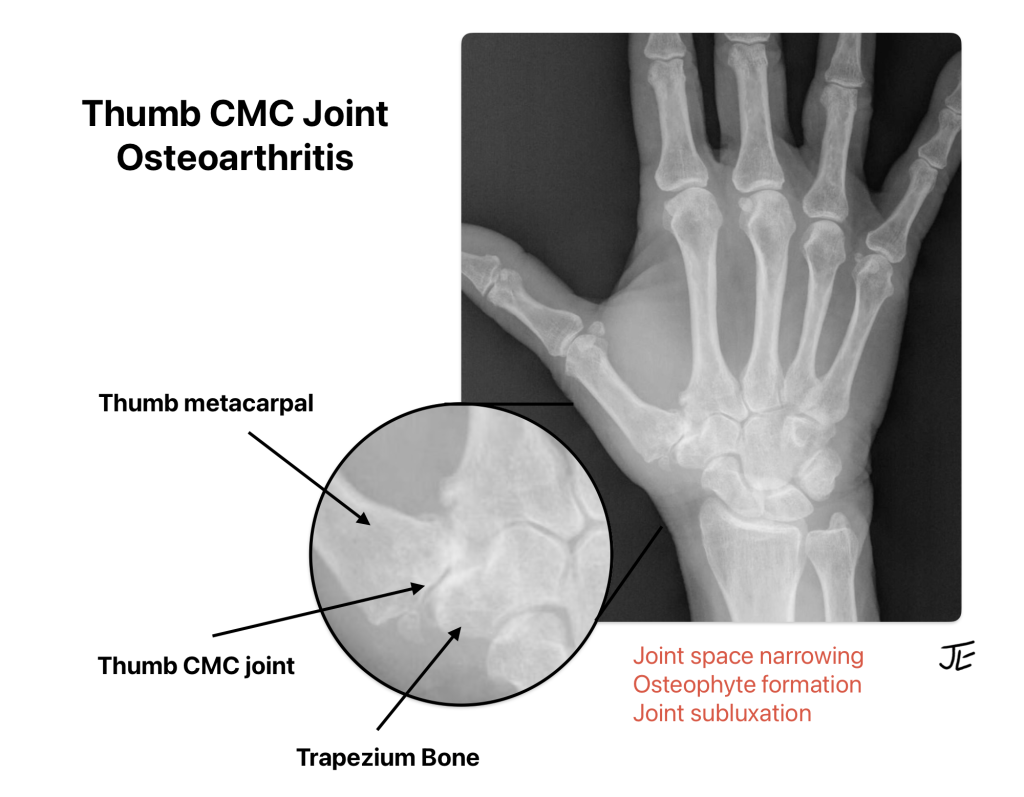
Thumb CMC joint osteoarthritis is very common, particularly among women over age 50. In many cases the arthritis pain is dull, achy, mild, and intermittent. In some cases, however, the condition can result in frequent episodes of severe pain, hand weakness, thumb deformity, and reduced quality of life. With severe thumb CMC joint osteoarthritis pain, simple fine motor tasks such as using a key or opening a medicine bottle can become impaired.
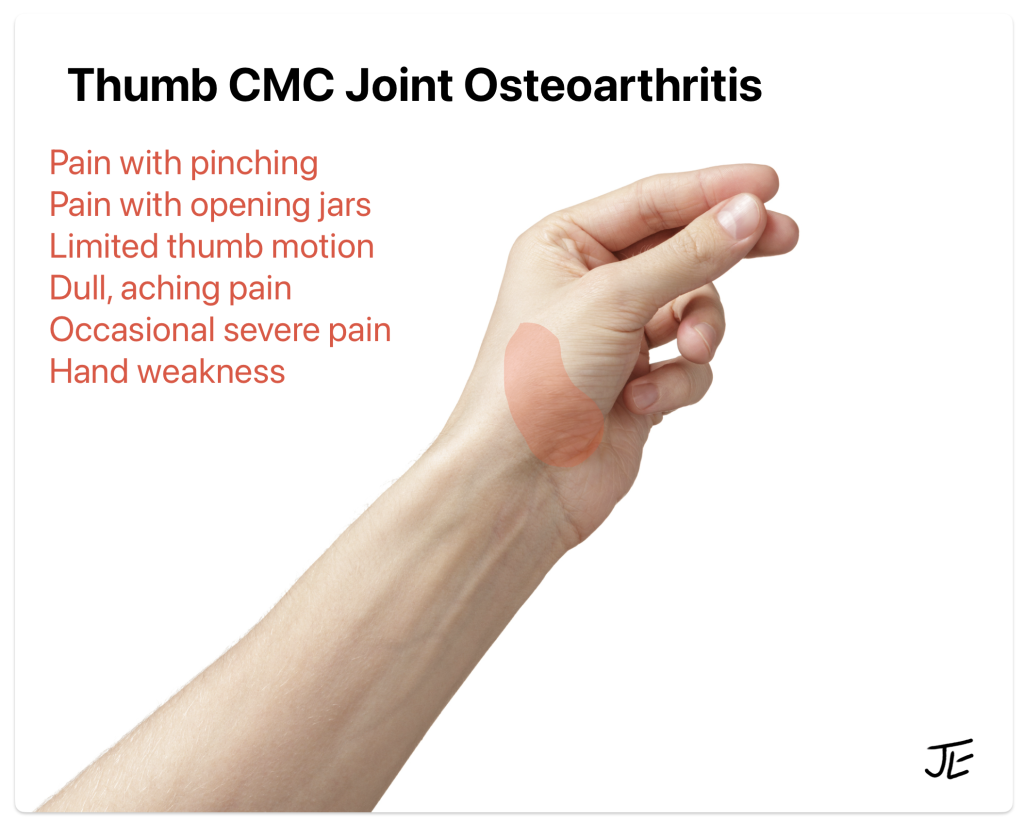
There are many treatments available for patients with thumb CMC joint osteoarthritis. First-line treatments include thumb splinting, activity modification, oral and topic NSAIDs, and hand therapy exercises. If these are not effective, many patients consider a corticosteroid injection to reduce pain and inflammation in the joint. In the majority of cases, nonsurgical treatment will control the symptoms reasonably well for patients. Therefore, most patients with thumb CMC joint osteoarthritis do not need surgery.
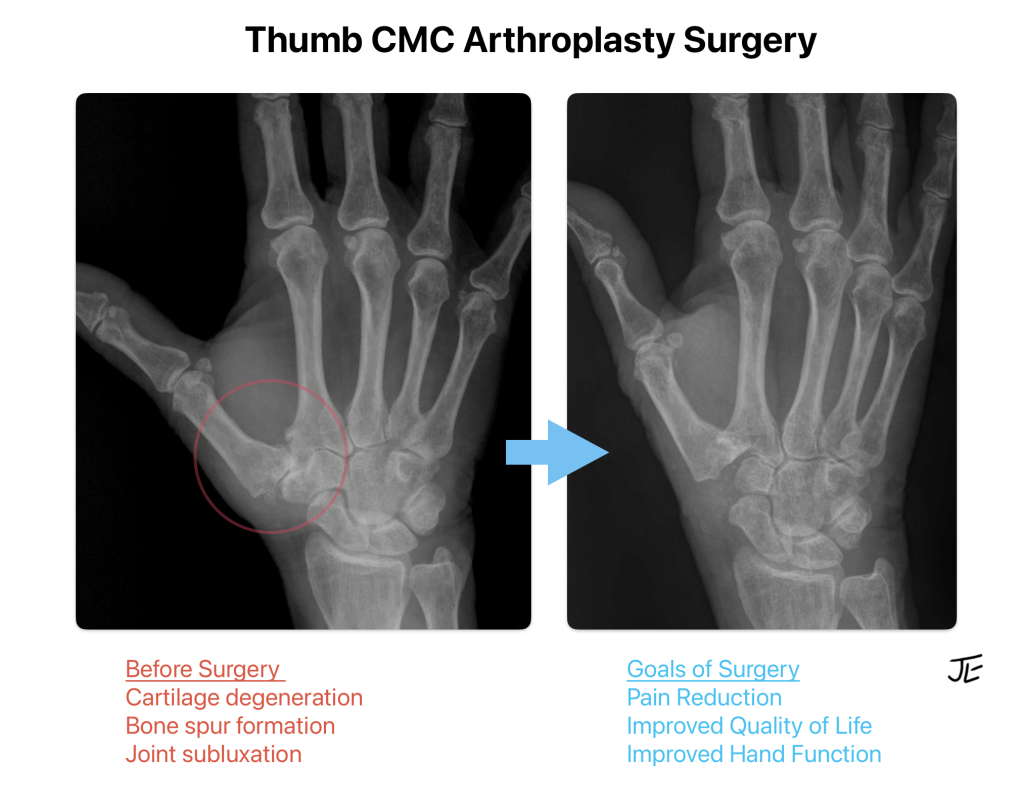
A patient may be a candidate for surgery if he or she has attempted nonsurgical treatment and yet continues to have significant thumb pain and reduced quality of life. The main goals of thumb arthritis surgery include pain relief, improved hand function, and improved quality of life. Secondary goals of surgery include improved thumb range of motion and improved grip and pinch strength.
What are the available surgical options for thumb CMC arthritis?
There are several options available for patients with thumb CMC joint osteoarthritis. Below are the most common procedures available:
Trapeziectomy. Most thumb arthritis surgeries begin with a trapeziectomy. This involves removal of the arthritic bone at the base of the thumb, called the trapezium. The suffix “ectomy” means surgical removal; for example, an appendectomy means removal of the appendix. This procedure was first performed in the 1940s and it is still considered to be very effective for patients. Removal of the arthritic trapezium bone is responsible for the pain relief experienced by patients. Due to the concern for instability of the base of the thumb following a trapeziectomy, most surgeons choose to stabilize the thumb, which can be performed in a number of ways, as listed below.
Thumb CMC Arthroplasty with ligament reconstruction and tendon interposition (LRTI). LRTI is the most commonly performed procedure for thumb CMC joint osteoarthritis in the United States today. This procedure was popularized in the 1980s. This surgery includes the trapeziectomy and the use of a patient’s forearm tendon to reconstruct the ligaments at the base of the thumb for added stability. The tendon can also be placed into the space left by the trapeziectomy to serve as a soft tissue cushion. There are no artificial implants required for the LRTI procedure. There are many studies showing good-to-excellent long-term results with this traditional procedure.
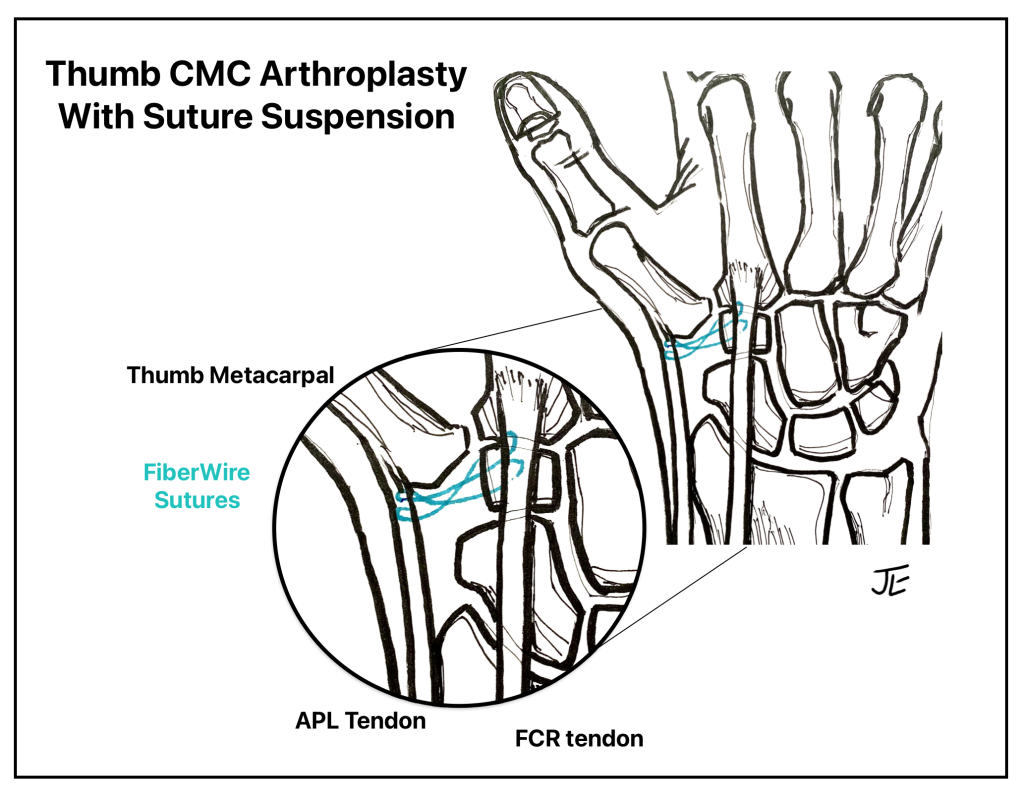
Thumb CMC Arthroplasty with Suture Suspension. Suture suspension is a newer technique which is becoming more popular as a less-invasive surgical option. After the trapeziectomy is performed, the surgeon uses strong sutures, often fiberwire, to stabilize the thumb base to the adjacent tendons. This technique does not require a drill hole in the bone or removal of a patient’s tendon. The procedure allows for early range of motion with hand therapy.
Thumb CMC Arthroplasty with Suture Button. Suture button reconstruction is another newer technique, which is often called tightrope reconstruction. After the trapeziectomy is performed, the surgeon inserts a strong suture device and a metallic button implant which is drilled into the metacarpal bone. This technique does not require removal of a patient’s tendon and it allows for early range of motion with hand therapy.
Thumb CMC Arthroplasty with Prosthetic Implant. Implant arthroplasty is less commonly performed in the United States than in Europe. This technique involves a small artificial implant made of metal or other synthetic material to create a new joint surface, once a partial or total trapeziectomy is performed. Surgeons who recommend this technique report good patient satisfaction as well as improved pinch strength and hand function. There are several implant designs on the market, but it is not clear which implant is superior. This procedure carries the unique risks of implant breakage, loosening, and implant rejection.
Thumb CMC joint fusion. Thumb CMC fusion or arthrodesis is rarely recommended due to the significant limitations in thumb mobility as a result of the surgery. This procedure is probably best suited for a young person who works a heavy manual labor job. Metal pins or plates and screws are used to fix the thumb CMC joint in a permanent position, which eliminates the joint pain, but also eliminates the joint motion.
What is the best surgery for thumb CMC arthritis?
The best surgery for thumb CMC arthritis is still controversial today. There are many types of surgeries available, as listed above, and this can seem overwhelming to patients. However, when a patient has severe arthritis pain in the joint, the most beneficial part of the surgery is removing the arthritic bone-on-bone at the base of the thumb.
Patient factors to consider before surgery include the patient’s age, activity level, functional demands, medical risk factors, and how the hand functions as a whole. Surgeons also consider the condition of other joints of the hand and thumb, including the STT joint and the thumb MP joint, when advising their patients.
The surgeon’s experience also plays a role in decision-making. It is important to consider what has worked well “in the surgeon’s hands.” Many surgeons have experience with one or two techniques and become very good at these procedures with each added repetition. Cost is another factor to consider in today’s healthcare environment, with implants resulting in a significant additional expense.
While I have performed the traditional LRTI procedure for many years with good results, I have begun using the newer, less-invasive suture suspension technique. I believe that this technique is less painful and allows for a quicker recovery, compared to the traditional thumb CMC surgery. The suture suspension technique also has a low risk of complications and positive long-term outcome data. Recently published studies show good-to-excellent functional results in patients up to 14 years after suture suspension surgery, with improved pinch strength and maintained pain relief. However, I advise patients that the procedure is not a “quick fix” as it takes about 3 months to return to heavy hand use and up to a year to obtain maximal thumb range of motion and pinch strength. I also recommend that patients attempt several months of nonsurgical treatment before considering surgery, since the symptoms may improve significantly without surgery.
Patients can trust the doctors and therapists at the Raleigh Hand to Shoulder Center to provide them with effective and compassionate care for their thumb CMC joint osteoarthritis.
Updated November 2025
Disclaimer: The information on this website is intended for general information only, and it does not constitute medical advice. This educational material does not replace an evaluation by a qualified medical professional. Please make an appointment with a physician if you have concerns.
